PaulSa, I don't know what you discussed with Dr. Potter and I'm not a medical doctor but here are some of my thoughts.
We don't know what the limit of detection of scar tissue is for the MRI so you might have scar tissue around the pudendal nerve, such as in the posterior aspect of the pudendal nerve, that just can't be seen. It is good news though that it appears that at least your pudendal nerve looks good until you get out to at the least the anterior portion of Alcock's canal and that it is really the branches of the pudendal nerve that appear to be the areas with scarring.
A varix is a dilated/swollen vein or artery. Since veins, arteries and nerves run together as a neurovascular bundle that evidence of a compressed nerve by scarring is a dilated vein because the vein is also compressed from the scarring. To me this suggest that you have some type of bilateral entrapment of the dorsal branch of the pudendal nerve since the report shows varices worse on the right then the left dorsal branch. This could easily explain the penile burning that you complain of. Do you have any ED symptoms (you don't have to answer if to personal).
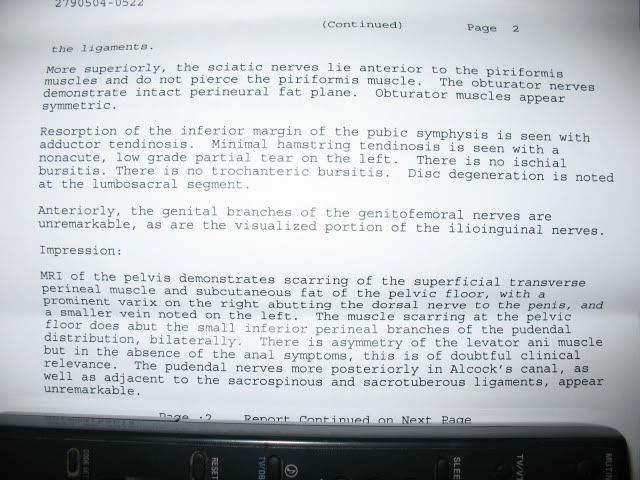
The perineal nerve branches and one of its branches is the posterior pudendal nerve which innervates the scrotum (see picture below). It seems possible to me that what Dr. Potter describes in the anteriorlateral margin of the levator ani muscle would account for the scrotal pain that you describe. Another possibility, since you don't complain of rectal pain, is that you have referred pain. There is evidence in other nerve conditions that the pain signal travels back up through the nerve and to another site and that is where the pain is felt.
Tendinosis is not the same as tendinitis and is a chronic change to the tendon due to muscle tears. Treatment options are limited and I commented on this on Mulan's MRI so I won't here.
Good luck with your next step and glad the MRI has information to help you move forward.

- Pudendal nerve
- Pudendal nerve male.png (102.64 KiB) Viewed 5436 times
2/07 LAVH and TOT 7/07 TOT right side removed 9/07 IL, IH and GN neuropathy 11/07 PN - Dr. Howard
6/08 Obturator neuralgia - Dr. Conway 11/08 Disability, piriformis syndrome - Dr. Howard
4/09 Bilateral obturator decompression surgery, BLL RSD - Dr. Howard
9/10 Removed left side TOT, botox, re-evaluate obturator nerve - Dr. Hibner
2/11 LFCN and saphenous neuralgia - Dr. Dellon 2/11 MRI with Dr. Potter - confirmed entrapment
5/11 Right side TG - Dr. Hibner 2012 Left side TG - Dr. Hibner